
 Copy to clipboard
Copy to clipboard 
Post-surgical infection control is a top priority in the reduction of complications, revisions and costs. It’s a topic of importance along the spectrum of development, from the research level, to start-up, through to the industry’s largest companies.
As the healthcare system navigates through rising costs and initiatives to maximize outcomes and patient satisfaction, manufacturers and researchers are betting on technologies to prevent infections following orthopaedic procedures—and for good reason. It’s an opportunity to provide surgeons, hospitals and most importantly, patients with the means to manage this burden.
Myriad studies and statistics cite how many infections occur, where, and how they’re financially impacting the healthcare system.
The data is compelling. But all of that aside, it should be clear that any infection is of concern, and thus, an area in need of solutions.
Of particular importance, according to one researcher, is that historically, cases of infections following orthopaedic procedures have been under- or mis-reported, masking the actual incidence levels.
“In the U.S., we have a reimbursement process that favors clinicians and hospitals to report a failed implant not due to infection,” says Thomas Webster, Ph.D., Chair and Professor of Chemical Engineering at Northeastern University. “The system says, if you have an infected implant, the hospital has to cover the cost. There are many cases in orthopaedics for which you could attribute a failed implant due to lack of bone growth, and that occurs. But one reason you could have that lack of bone growth is infection.”
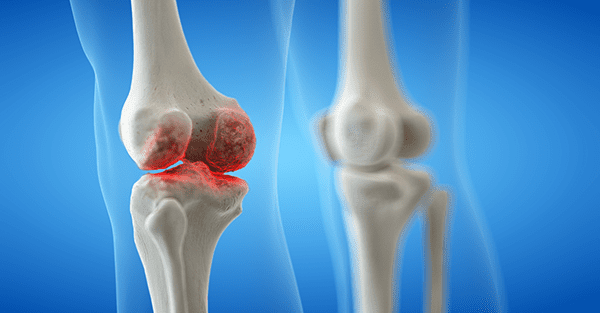
The issue is not limited to one market segment in the orthopaedic industry either, though some may be harder to manage—for instance in spine, where a patient is exposed for long periods of time, and trauma because of the unexpected nature of those cases.
Again, regardless of the frequency or costs, it seems that industry agrees that one infection is too many, as demonstrated by the introduction of new approaches to prevent infections.
There’s a variety of options. Some manufacturers are applying antibiotic coatings or modifying surfaces through nanotechnology, while others deliver antibiotics through bone substitute materials. Some are focusing on disposables and sterile instruments.
Of these, all but disposables and sterile instruments are still in the early development stages. Here, we examine some of these approaches.
New Technology
PolyPid is conducting a clinical trial of BonyPid-1000™, described by the company as a drug/device combination containing tri-calcium phosphate bone void filler and the company’s PLEX platform technology. The PLEX encapsulation matrix contains an antibiotic that is released locally over 30 days, says Dikla Czaczkes Akselbrad, PolyPid’s Chief Strategy Officer.
The BonyPid approach combines four attributes: local administration, a broad spectrum antibiotic, pre-determined and prolonged periods of release and a small, safe overall dose that generates high local concentration.
Local administration plays a particularly important role in this approach, Czaczkes Akselbrad says.
“The standard of care includes systemic administration [of antibiotics into the bone void], which is limited due to low penetration into the needed site. Local delivery may overcome this issue. However, the approved local solutions are characterized by short-term and non-controlled release of the entrapped drug,” she says.
“Currently, in the U.S., the only approved local delivery is based on a cement polymer that releases an effective amount of antibiotics over a short period (several days), which is also characterized by high burst release. This release profile is limited in the eradication of significant bacterial load, and can even lead to resistant strains of bacteria.”
BonyPid-1000 is undergoing a pivotal clinical study for CE Mark approval, and PolyPid plans to submit an IDE by the end of 2016 for further FDA approval.
Another approach to preventing infections in trauma is employed by Silver Bullet Therapeutics’ OrthoFuzIon Antimicrobial Bone Screw, which uses an electrical charge to release a cloud of antimicrobial silver ions around the implanted device. The product received its CE Mark in March 2015, and FDA approval is expected in 2016.
The system is powered by a self-sustaining battery that co-sputters silver with platinum to release silver ions into the local area around the implant, creating that cloud of anti-infectivity, according to Paul Chirico, Co-Founder, President and CEO of Silver Bullet Therapeutics.
Chirico notes the challenges and twofold implication of silver.
“The wonderful thing about silver is, it’s localized, so it stays where you need it,” he says. “That’s also the bad thing about silver. It’s not a systemic, unlike some companies that have gone in the direction of antibiotics, which are systemic and have tremendous hypersensitivities associated with them.”
Tyber Medical worked with Dr. Webster to develop its process to prevent infections. Tyber Medical is using nanotechnology with its BioTy™ Modified Surface Treatment, which can be applied to titanium, stainless steel, cobalt chrome and PEEK. The surface modification process creates a texture designed to be a bacteriostatic surface to reduce the adhesion of bacteria and biofilm formation.
Tyber Medical has received two FDA 510(k) clearances for BioTy on the company’s headed, headless and snap-off screw systems. They are currently working through the FDA process to establish enhanced claims and are planning a limited launch by 2016’s end.
Webster has studied the use of ceramic nanomaterials to control surface energy to decrease infection, promote bone growth and inhibit inflammation.
“Nanotechnology allows you to increase the surface area of your implant. So if you took a ceramic implant and made it out of nanomaterials, you’d have much more surface energy,” he says. “That allows you to control the charge of your surface, which also allows you to increase the absorption of things like LubriSyn, so you can keep that ceramic from becoming infected.”
Webster worked with Amedica a few years ago, and merged this concept with their silicon nitride technology in spine.
“[Amedica] submitted this to FDA to get an expanded claim on their silicon nitride material to reduce infections, without using antibiotics, through this nanotechnology approach,” Webster says. “In three months, FDA allowed them to expand their claim to reduce infection.
“If you keep the chemistry the same, and only change nanotechnology (the surface area which will change the charge of your material), you can tell FDA that you’re implanting the same thing that’s been implanted for decades; you just want to change the roughness at the nanoscale to get these attractive properties. That has allowed for very quick FDA approval.”
Future Technology
Dr. Webster is particularly enthusiastic about the possibilities of implanted sensors that can communicate to surgeons whether an infection is forming—an idea that may be only five years from prototype and testing.
“On some hip implants, we’re making sensors out of nanomaterials and ceramics that can sense, in real time, what’s occurring so that the surgeon can intervene quicker—so you don’t get a biofilm forming and don’t have to remove the implant,” he says. “These earlier intervention strategies are dependent upon sensors. We have a sensor to measure cellular events in real time, and an approach that you can apply an electromagnetic field if you know bacteria are on the implant, to kill them. But, we haven’t figured out [how to power this]. Implant companies we’ve talked to are not excited about putting a battery in their implant, and manufacturing that for a hip implant would be expensive. I think a lot of companies don’t even want to go there.
“We also have to figure out how to develop the sensor so that it can communicate to a computer or handheld device outside the body. We don’t think that’s a big issue, we think we can do that; we just get so excited when we think about the day that you can insert a hip implant into a patient, and the minute after it’s inserted, you can collect all of this data on what kind of cells are attaching, how many cells are attaching and are you headed down the road for success or for infection or scar tissue growth? We might then have an earlier intervention to keep that from happening.”
The Challenges
Not surprisingly, each company employing or developing these new technologies has arguments for their approach and against other routes.
Silver Bullet Therapeutics’ leadership, for example, is skeptical that coatings can prevent infections.
“You could take an antibiotic and paint it on, which sounds like a great idea, but it really isn’t,” says Bohdan Chopko, M.D., Ph.D., Co-Founder of Silver Bullet Therapeutics and Associate Professor of Neurosurgery for Stanford University. “The antibiotic-coated device idea has a lot of issues, from patient sensitivity to antibiotics, to controlling the release, to having it scrape off if you’re placing a screw into bone.”
There are distinct issues with technologies that elute a pharmacological drug or a metal ion, versus technologies that modify surfaces, says Rui Ferreira, Vice President of Research & Development at Tyber Medical.
“The challenge is that either one of those will work for a time, but a dose response dilution will be associated,” he says. “It’s going to start off having an effect, but will change over time because as it elutes, it leaches off and that causes challenges from FDA.”
Webster and Ferreira agree that antibiotics aren’t cutting it and may be breeding resistant strains of infections.
“The challenge with orthopaedic implants is that once bacteria colonizes on implants and forms biofilms, regular pharmaceutical treatments can’t eradicate the infection; you can’t get it killed and cleaned off of the implant,” Ferreira says.
The widespread production, use and misuse of antibiotics have contributed to the next generation of drug resistant infectious organisms, commonly called superbugs.
“The problem is that we thought antibiotics would be the solution, so that was really the only approach. We know now that doesn’t work,” Webster says.
New chemistries are emerging to kill bacteria and increase bone growth, such as selenium, though they would likely take over a decade for FDA to approve, Webster says.
Conclusion
It is too early to name the most effective approach for preventing infections. As previously mentioned, many companies are focused on the topic and some are pursuing coatings or disposables. For example, Stryker recently spent $2.7 billion to acquire Sage Products, a developer and manufacturer of disposable products targeted to reduce “Never Events.” In 2015, DePuy Synthes mentioned infection control as a priority, but gave little detail.
More infection prevention research is a step in the right direction, Webster says, adding, “Even if it fails, at least there are more people looking at orthopaedic implant infections.”
He does point out the potential toxicity in materials like silver, copper or zinc.
“You have to be careful of the concentration you’re using and make sure that whatever the element is, you’re killing bacteria or keeping them from attaching at that concentration,” Webster says. “Some of the new chemistries I’ve seen have a high toxicity profile to osteoblasts. They may kill bacteria too, but unfortunately they also keep bone from growing.”
The issue of whether or not hospitals and surgery centers will actually pay for new technologies and cutting-edge devices, like sensors, will ultimately depend on long-term outcomes to demonstrate cost savings. Companies commercializing these technologies argue that if a certain patient population is prone to infection, a higher price might be justified if the technology can prevent infection.
“As researchers, we can do a better job of explaining to the hospitals that even though what we’re developing now is more expensive, look at the long-term data: in reducing return visits, returning high quality of life and having the ability to say to patients, ‘Come here to get your surgery done because we’re employing the highest performing implants’ – with long-term data, maybe those arguments would be made solid,” Webster says.
Post-surgical infection control is a top priority in the reduction of complications, revisions and costs. It’s a topic of importance along the spectrum of development, from the research level, to start-up, through to the industry’s largest companies.
As the healthcare system navigates through rising costs and initiatives to maximize outcomes...
Post-surgical infection control is a top priority in the reduction of complications, revisions and costs. It’s a topic of importance along the spectrum of development, from the research level, to start-up, through to the industry’s largest companies.
As the healthcare system navigates through rising costs and initiatives to maximize outcomes and patient satisfaction, manufacturers and researchers are betting on technologies to prevent infections following orthopaedic procedures—and for good reason. It’s an opportunity to provide surgeons, hospitals and most importantly, patients with the means to manage this burden.
Myriad studies and statistics cite how many infections occur, where, and how they’re financially impacting the healthcare system.
The data is compelling. But all of that aside, it should be clear that any infection is of concern, and thus, an area in need of solutions.
Of particular importance, according to one researcher, is that historically, cases of infections following orthopaedic procedures have been under- or mis-reported, masking the actual incidence levels.
“In the U.S., we have a reimbursement process that favors clinicians and hospitals to report a failed implant not due to infection,” says Thomas Webster, Ph.D., Chair and Professor of Chemical Engineering at Northeastern University. “The system says, if you have an infected implant, the hospital has to cover the cost. There are many cases in orthopaedics for which you could attribute a failed implant due to lack of bone growth, and that occurs. But one reason you could have that lack of bone growth is infection.”
The issue is not limited to one market segment in the orthopaedic industry either, though some may be harder to manage—for instance in spine, where a patient is exposed for long periods of time, and trauma because of the unexpected nature of those cases.
Again, regardless of the frequency or costs, it seems that industry agrees that one infection is too many, as demonstrated by the introduction of new approaches to prevent infections.
There’s a variety of options. Some manufacturers are applying antibiotic coatings or modifying surfaces through nanotechnology, while others deliver antibiotics through bone substitute materials. Some are focusing on disposables and sterile instruments.
Of these, all but disposables and sterile instruments are still in the early development stages. Here, we examine some of these approaches.
New Technology
PolyPid is conducting a clinical trial of BonyPid-1000™, described by the company as a drug/device combination containing tri-calcium phosphate bone void filler and the company’s PLEX platform technology. The PLEX encapsulation matrix contains an antibiotic that is released locally over 30 days, says Dikla Czaczkes Akselbrad, PolyPid’s Chief Strategy Officer.
The BonyPid approach combines four attributes: local administration, a broad spectrum antibiotic, pre-determined and prolonged periods of release and a small, safe overall dose that generates high local concentration.
Local administration plays a particularly important role in this approach, Czaczkes Akselbrad says.
“The standard of care includes systemic administration [of antibiotics into the bone void], which is limited due to low penetration into the needed site. Local delivery may overcome this issue. However, the approved local solutions are characterized by short-term and non-controlled release of the entrapped drug,” she says.
“Currently, in the U.S., the only approved local delivery is based on a cement polymer that releases an effective amount of antibiotics over a short period (several days), which is also characterized by high burst release. This release profile is limited in the eradication of significant bacterial load, and can even lead to resistant strains of bacteria.”
BonyPid-1000 is undergoing a pivotal clinical study for CE Mark approval, and PolyPid plans to submit an IDE by the end of 2016 for further FDA approval.
Another approach to preventing infections in trauma is employed by Silver Bullet Therapeutics’ OrthoFuzIon Antimicrobial Bone Screw, which uses an electrical charge to release a cloud of antimicrobial silver ions around the implanted device. The product received its CE Mark in March 2015, and FDA approval is expected in 2016.
The system is powered by a self-sustaining battery that co-sputters silver with platinum to release silver ions into the local area around the implant, creating that cloud of anti-infectivity, according to Paul Chirico, Co-Founder, President and CEO of Silver Bullet Therapeutics.
Chirico notes the challenges and twofold implication of silver.
“The wonderful thing about silver is, it’s localized, so it stays where you need it,” he says. “That’s also the bad thing about silver. It’s not a systemic, unlike some companies that have gone in the direction of antibiotics, which are systemic and have tremendous hypersensitivities associated with them.”
Tyber Medical worked with Dr. Webster to develop its process to prevent infections. Tyber Medical is using nanotechnology with its BioTy™ Modified Surface Treatment, which can be applied to titanium, stainless steel, cobalt chrome and PEEK. The surface modification process creates a texture designed to be a bacteriostatic surface to reduce the adhesion of bacteria and biofilm formation.
Tyber Medical has received two FDA 510(k) clearances for BioTy on the company’s headed, headless and snap-off screw systems. They are currently working through the FDA process to establish enhanced claims and are planning a limited launch by 2016’s end.
Webster has studied the use of ceramic nanomaterials to control surface energy to decrease infection, promote bone growth and inhibit inflammation.
“Nanotechnology allows you to increase the surface area of your implant. So if you took a ceramic implant and made it out of nanomaterials, you’d have much more surface energy,” he says. “That allows you to control the charge of your surface, which also allows you to increase the absorption of things like LubriSyn, so you can keep that ceramic from becoming infected.”
Webster worked with Amedica a few years ago, and merged this concept with their silicon nitride technology in spine.
“[Amedica] submitted this to FDA to get an expanded claim on their silicon nitride material to reduce infections, without using antibiotics, through this nanotechnology approach,” Webster says. “In three months, FDA allowed them to expand their claim to reduce infection.
“If you keep the chemistry the same, and only change nanotechnology (the surface area which will change the charge of your material), you can tell FDA that you’re implanting the same thing that’s been implanted for decades; you just want to change the roughness at the nanoscale to get these attractive properties. That has allowed for very quick FDA approval.”
Future Technology
Dr. Webster is particularly enthusiastic about the possibilities of implanted sensors that can communicate to surgeons whether an infection is forming—an idea that may be only five years from prototype and testing.
“On some hip implants, we’re making sensors out of nanomaterials and ceramics that can sense, in real time, what’s occurring so that the surgeon can intervene quicker—so you don’t get a biofilm forming and don’t have to remove the implant,” he says. “These earlier intervention strategies are dependent upon sensors. We have a sensor to measure cellular events in real time, and an approach that you can apply an electromagnetic field if you know bacteria are on the implant, to kill them. But, we haven’t figured out [how to power this]. Implant companies we’ve talked to are not excited about putting a battery in their implant, and manufacturing that for a hip implant would be expensive. I think a lot of companies don’t even want to go there.
“We also have to figure out how to develop the sensor so that it can communicate to a computer or handheld device outside the body. We don’t think that’s a big issue, we think we can do that; we just get so excited when we think about the day that you can insert a hip implant into a patient, and the minute after it’s inserted, you can collect all of this data on what kind of cells are attaching, how many cells are attaching and are you headed down the road for success or for infection or scar tissue growth? We might then have an earlier intervention to keep that from happening.”
The Challenges
Not surprisingly, each company employing or developing these new technologies has arguments for their approach and against other routes.
Silver Bullet Therapeutics’ leadership, for example, is skeptical that coatings can prevent infections.
“You could take an antibiotic and paint it on, which sounds like a great idea, but it really isn’t,” says Bohdan Chopko, M.D., Ph.D., Co-Founder of Silver Bullet Therapeutics and Associate Professor of Neurosurgery for Stanford University. “The antibiotic-coated device idea has a lot of issues, from patient sensitivity to antibiotics, to controlling the release, to having it scrape off if you’re placing a screw into bone.”
There are distinct issues with technologies that elute a pharmacological drug or a metal ion, versus technologies that modify surfaces, says Rui Ferreira, Vice President of Research & Development at Tyber Medical.
“The challenge is that either one of those will work for a time, but a dose response dilution will be associated,” he says. “It’s going to start off having an effect, but will change over time because as it elutes, it leaches off and that causes challenges from FDA.”
Webster and Ferreira agree that antibiotics aren’t cutting it and may be breeding resistant strains of infections.
“The challenge with orthopaedic implants is that once bacteria colonizes on implants and forms biofilms, regular pharmaceutical treatments can’t eradicate the infection; you can’t get it killed and cleaned off of the implant,” Ferreira says.
The widespread production, use and misuse of antibiotics have contributed to the next generation of drug resistant infectious organisms, commonly called superbugs.
“The problem is that we thought antibiotics would be the solution, so that was really the only approach. We know now that doesn’t work,” Webster says.
New chemistries are emerging to kill bacteria and increase bone growth, such as selenium, though they would likely take over a decade for FDA to approve, Webster says.
Conclusion
It is too early to name the most effective approach for preventing infections. As previously mentioned, many companies are focused on the topic and some are pursuing coatings or disposables. For example, Stryker recently spent $2.7 billion to acquire Sage Products, a developer and manufacturer of disposable products targeted to reduce “Never Events.” In 2015, DePuy Synthes mentioned infection control as a priority, but gave little detail.
More infection prevention research is a step in the right direction, Webster says, adding, “Even if it fails, at least there are more people looking at orthopaedic implant infections.”
He does point out the potential toxicity in materials like silver, copper or zinc.
“You have to be careful of the concentration you’re using and make sure that whatever the element is, you’re killing bacteria or keeping them from attaching at that concentration,” Webster says. “Some of the new chemistries I’ve seen have a high toxicity profile to osteoblasts. They may kill bacteria too, but unfortunately they also keep bone from growing.”
The issue of whether or not hospitals and surgery centers will actually pay for new technologies and cutting-edge devices, like sensors, will ultimately depend on long-term outcomes to demonstrate cost savings. Companies commercializing these technologies argue that if a certain patient population is prone to infection, a higher price might be justified if the technology can prevent infection.
“As researchers, we can do a better job of explaining to the hospitals that even though what we’re developing now is more expensive, look at the long-term data: in reducing return visits, returning high quality of life and having the ability to say to patients, ‘Come here to get your surgery done because we’re employing the highest performing implants’ – with long-term data, maybe those arguments would be made solid,” Webster says.

You are out of free articles for this month
Subscribe as a Guest for $0 and unlock a total of 5 articles per month.
You are out of five articles for this month
Subscribe as an Executive Member for access to unlimited articles, THE ORTHOPAEDIC INDUSTRY ANNUAL REPORT and more.
HC
Hannah Corcoran is an Associate Editor at ORTHOWORLD.